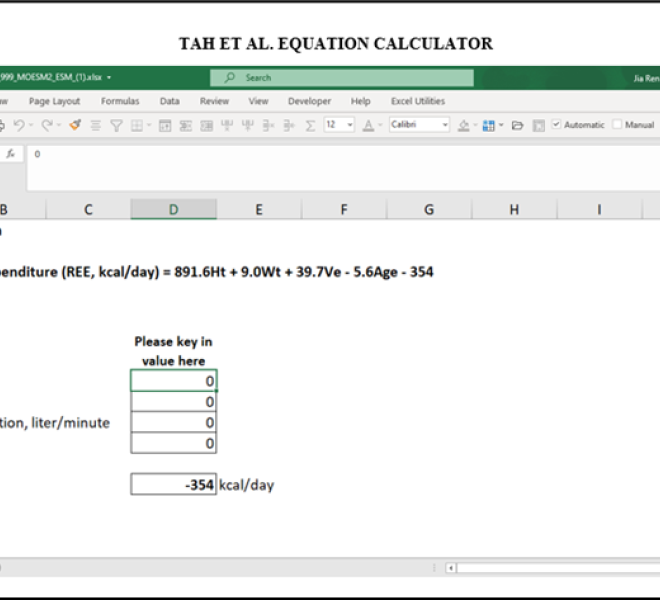
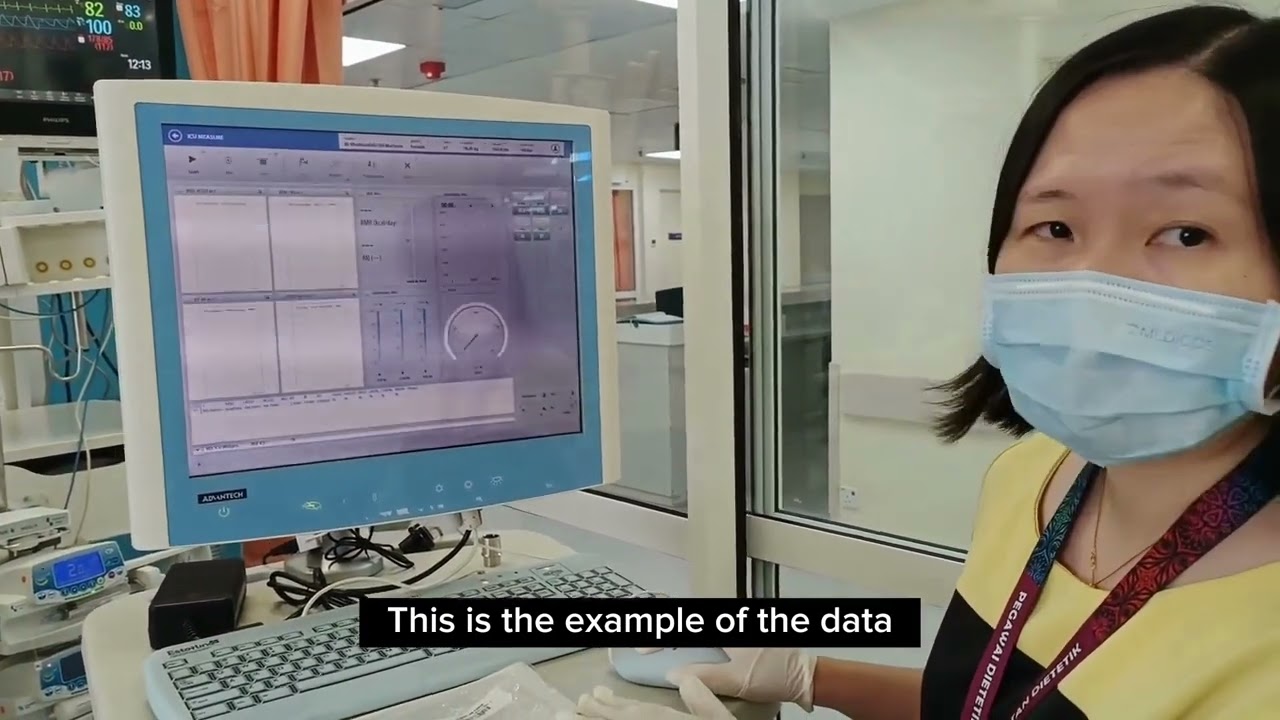
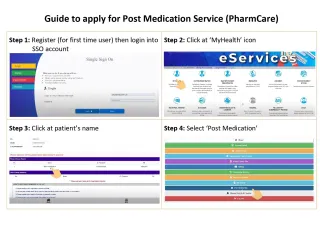
This innovation project aims to develop a more accurate predictive equation (PE) for estimating resting energy expenditure (REE) in Asian critically ill patients when indirect calorimetry (IC) is not available. IC was used to measure REE at acute (≤5 days; n = 294) and late (≥6 days; n = 180) phases of intensive care unit (ICU) admission. Two PEs developed from paired 168-patient data were compared with measured REE using mean absolute percentage difference (MSPD). We have employed a unique 2-step design to confirm whether two PEs are needed for the acute and late phases of critical illness. We a priori set a 20% MSPD threshold based on the PermiT trial. We decided that only one PE was needed after we found that the MSPD was <20% between the two phases. PEs were developed by multiple linear regression. Subsequently, multi-fold cross-validation approach was used to validate the developed PEs. The best PEs were selected based on the highest coefficient of determination (R2), the lowest root mean square error (RMSE) and the lowest standard error of estimate (SEE). The first and best PE was developed and validated for the estimation of REE in both acute and late phases. The novel PE(Tah et al. equation) is [891.6 (Height in m) + 9.0 (Weight in kg) + 39.7 (Minute Ventilation in L/min) − 5.6 (Age) − 354], with R2 = 0.442, RMSE = 348.3, SEE = 325.6 and MSPD with measured REE was: 15.1 ± 14.2% [acute], 15.0 ± 13.1% [late]. This PE has been converted into software (Microsoft Excel Tah et al. equation calculator) for the estimation of REE and to optimize nutrition intake among Asian critically ill patients. [Published in Tah et al. (2021) European Journal of Clinical Nutrition[3] (Refer Appendix A)] This project showed no significant association between <80% or ≥80% of goal-directed energy and protein adequacy with mortality outcomes and quality of life. But overfeeding in the acute phase is significantly associated with unfavourable outcomes such as increased ICU length of stay (LOS) with average 3 days longer LOS, increased hospital LOS with average 7 days longer LOS, reduced 28-day and 60-day ventilator-free days, and associated with early (<7 days) healthcare-associated infection (p<0.05). Consequently, this project suggests being conservative with energy and protein provision (60 – 80% goal) during the acute phase and progression to full goal-directed energy and protein (80 – 100% goal) after the acute phase of critical illness is prudent for patient recovery. Implementing individualized energy requirement equations when IC is unavailable can lead to significant benefits, including estimated cost savings of RM4,507,200.00 per year, reduced adverse outcomes such as LOS, length of ventilation, malnutrition rates, and infection, and improved patient recovery. The findings have the potential to update clinical practice guidelines and enhance nutrition support management in the ICU setting. Currently, Tah et al. equation was used in the Comparative Standards in the iPesakit System UMMC to calculate energy requirements for ventilated ICU patients before nutrition intervention done by dietitians in UMMC. Acknowledgement: FRGS/1/2018/SKK02/UM/02/3 FP003-2018A.




Comment